Bacterial keratitis
Bacterial keratitis usually develops only ocular defences are compromised .
• Pseudomonas aeruginosa may be a ubiquitous Gram-negative bacillus (rod) commensal of the alimentary canal . The infection is usually aggressive and is liable for over 60% of contact lens-related keratitis.
• Staphylococcus aureus may be a common Gram-positive and coagulase-positive commensal of the nares, skin and conjunctiva. Keratitis tends to present with a focal and fairly well-defined white or yellow–white infiltrate.
• Streptococci. S. pyogenes may be a common Gram-positive commensal of the throat and vagina. S. pneumonia (pneumococcus) may be a Gram-positive commensal of the upper tract . Infections with streptococci are often aggressive.
Risk factors
• contact wear, particularly if extended, is that the most vital risk factor. Corneal epithelial compromise secondary to hypoxia and minor trauma is assumed to be important, as is bacterial adherence to the lens surface.
Wearers of sentimental lenses are at higher risk than those of rigid gas permeable and other types. Infection is more likely if there's poor lens hygiene but it also can occur even with apparently meticulous lens care, and with daily disposable lenses.
• Trauma, including refractive surgery (particularly LASIK
– laser-assisted in place keratomileusis), has been linked to bacterial infection, including with atypical mycobacteria. In developing countries agricultural injury is that the major risk factor,
when mycosis should be considered.
• Ocular surface disease like herpetic keratitis, bullous keratopathy, dry eye, chronic blepharitis, trichiasis and entropion, exposure, severe allergic disease and corneal anaesthesia.
• Other factors include local or systemic immunosuppression, diabetes and vitaminA deficiency.
Clinical features
• Presentation is with pain, photophobia, blurred vision and
mucopurulent or purulent discharge.
• Signs
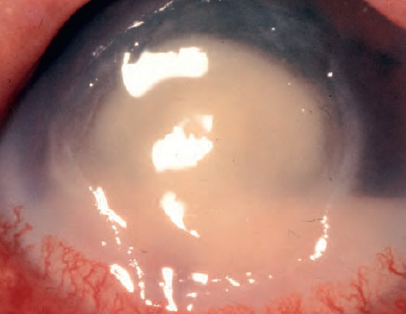
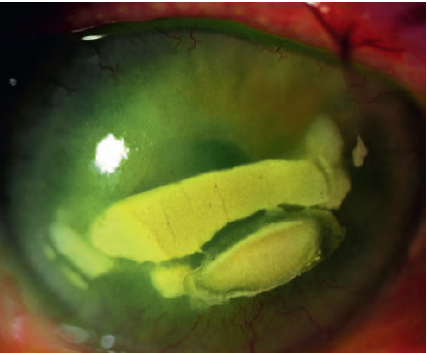
○ An epithelial defect with infiltrate involving a bigger area, and significant circum corneal injection.
○ Stromal oedema, folds in Descemet membrane and anterior uveitis, commonly with a hypopyon and posterior synechiae in moderate–severe keratitis.
Plaque-like keratic precipitates can form on the endothelium contiguous with the affected stroma.
○ Chemosis and eyelid swelling in moderate–severe cases.
○ Severe ulceration may cause descemetocoele formation and perforation, particularly in Pseudomonas infection.
○ Scleritis can develop, particularly with severe perilimbal infection.
○ Endophthalmitis is rare within the absence of perforation.
○ Improvement is typically heralded by a discount in eyelid oedema and chemosis, shrinking of the epithelial defect, decreasing infiltrate density and a discount in anterior chamber signs.
○ Subsequent scarring could also be severe, including vascularization; additionally to opacification irregular astigmatism may limit vision.
• Reduced corneal sensation may suggest associated neurotrophic keratopathy, particularly where there's no other major risk factor. Sensation can also be reduced in chronic surface disease, herpetic keratitis and long-term contact wear.
• IOP should be monitored
• medical diagnosis includes keratitis thanks to other microorganisms (fungi, acanthamoeba, stromal herpes simplex keratitis and mycobacteria), marginal keratitis, sterile inflammatory corneal infiltrates related to contact wear, peripheral ulcerative keratitis and toxic keratitis.
Investigations
• Corneal scraping. this might not be required for alittle infiltrate, particularly one without an epithelial defect and faraway from the visual axis.
○ A non-preserved local anesthetic is instilled (preservatives may lower bacterial viability for culture); one drop of proxymetacaine 0.5% is typically sufficient; tetracaine may have a greater bacteriostatic effect.
○ Scrapings are taken either with a disposable scalpel blade, the bent tip of a bigger diameter needle , or a sterile spatula.
○ the simplest thanks to ‘plate’ scrapings without breaking the gel surface is with a spatula. If a fresh spatula isn't available for every sample one instrument should be flame-sterilized between scrapes. Alternatively, a fresh scalpel blade or needle are often used for every pass. Calcium alginate swabs can also be satisfactory.
○ Loose mucus and necrotic tissue should be faraway from the surface of the ulcer before scraping.
○ The margins and base of the lesion are scraped.
○ a skinny smear is placed on one or two glass slides for microscopy, including Gram's method . A surface is provided on one side of 1 end of the slide for pencil labelling. The sample is allowed to dry during a ir at temperature for several minutes then placed in a slide carrier.
○ Re-scraping is performed for every medium and samples are plated onto culture media, taking care to not break the surface of the gel.
○ Routinely, blood, chocolate and Sabouraud media are used initially and therefore the samples are placed in an incubator until transported to the laboratory.
Refrigerated media should be gently warmed to temperature before sample application.
○ A blade or needle are often placed directly into bottled media like brain–heart infusion (BHI). there's evidence that one scrape, sent in BHI to the laboratory where it's homogenized and plated, provides similar results to the normal multi-scrape method.
○ Scraping could also be delayed without treatment for 12 hours if antibiotics have previously been commenced.
• Conjunctival swabs could also be worthwhile additionally to corneal scraping, particularly in severe cases, as occasionally an organism could also be cultured when a corneal scrape is negative. cotton , calcium alginate and artificial swabs have all been found to possess some bacteriostatic effect.
• contact cases, also as bottles of solution and lenses themselves, should be obtained when possible and sent to the laboratory for culture. The case shouldn't be cleaned by the patient first!
• Gram staining
○ Differentiates bacterial species into ‘Gram-positive’ and ‘Gram-negative’ supported the power of the dye to penetrate the cell membrane .
○ Bacteria that take up gentian violet are Gram-positive and people that allow the dye to scrub off are Gram-negative.
○ Other stains, generally not requested at initial investigation, are listed in.
• Culture and sensitivity reports should be obtained as soon as possible. the sort of bacteria alone will generally provide a sign of the antibiotic category to be used.
Treatment
General considerations
• Hospital admission should be considered for patients who aren't likely to comply or are unable to self-administer treatment. It should even be considered for aggressive disease, particularly if involving an only eye.
• Discontinuation of contact wear is mandatory.
• a transparent plastic eye shield should be worn between eye drop instillation if significant thinning is present.
• Decision to treat
○ Intensive treatment might not be required for little infiltrates that are clinically sterile and should be treated by lower-frequency topical antibiotic and/or steroid, and by temporary cessation of contact wear.
○ it's important to notice that the causative organism can't be defined reliably from the ulcer’s appearance.
○ Empirical broad-spectrum treatment is typically initiated before microscopy results are available.
Local therapy
Topical therapy are able to do high tissue concentration and initially should contains broad-spectrum antibiotics that cover commonest pathogens. Initially instillation is at hourly intervals day and night for 24–48 hours, then is tapered consistent with clinical progress.
• Antibiotic monotherapy has the main advantage over duotherapy of lower surface toxicity, also as greater convenience.
○ A commercially available fluoroquinolone is that the usual choice for empirical monotherapy and appears to be about as effective as duotherapy.
. Moxifloxacin, gatifloxacin and besifloxacin are new generation fluoroquinolones that largely address this, and even have better activity against Gram-positive pathogens.
Moxifloxacin has superior ocular penetration. Novel drug preparations, with higher concentrations or modified vehicles, are introduced to reinforce antibacterial activity.
○ Ciprofloxacin instillation is related to white corneal precipitates which will delay epithelial healing.
• Antibiotic duotherapy could also be preferred as first-line empirical treatment in aggressive disease or if microscopy suggests streptococci or a selected microorganism which will be more effectively treated by a tailored regimen.
○ Empirical duotherapy usually involves a mixture of two fortified antibiotics, typically a cephalosporin and an aminoglycoside, so as to hide common Grampositive and Gram-negative pathogens.
○ The antibiotics aren't commercially available and must be specially prepared. a typical parenteral or lyophilized antibiotic preparation is combined with a compatible vehicle such the antibiotic doesn't precipitate. Optimally, constitution should happen within the sterile preparation area of a pharmaceutical
○ Disadvantages of fortified antibiotics include high cost, limited availability, contamination risk, short shelf-life and therefore the need for refrigeration.
• Subconjunctival antibiotics are usually only indicated if there's poor compliance with topical treatment.
• Mydriatics (cyclopentolate 1%, homatropine 2% or atropine
1%) are wont to prevent the formation of posterior synechiae and to scale back pain.
• Steroids
○ Steroids reduce host inflammation, improve comfort, and minimize corneal scarring. However, they promote replication of some microorganisms, particularly fungi, herpes simplex and mycobacteria and are contraindicated if a fungal or mycobacterial agent is suspected.
By suppressing inflammation, they also retard the eye’s response to bacteria and this will be clinically significant, particularly if an antibiotic is of limited effect or bacteriostatic instead of bactericidal.
○ Evidence that they improve the ultimate visual outcome is especially empirical, but the recent Steroids for Corneal Ulcers Trial found no eventual benefit in most cases, though severe cases attended do better; a positive culture result was an inclusion criterion, and steroids were introduced after 48 hours of moxifloxacin.
○ Epithelialization could also be retarded by steroids and that they should be avoided if there's significant thinning or delayed epithelial healing; corneal melting can occasionally be precipitated or worsened.
○ Many authorities don't commence topical steroids until evidence of clinical improvement is seen with antibiotics alone, typically 24–48 hours after starting treatment.
Others delay their use a minimum of until the sensitivity of the isolate to antibiotics has been demonstrated, or don't use them in the least .
○ Regimens vary from minimal strength preparations at low frequency to dexamethasone 0.1% every 2 hours; an inexpensive regimen is prednisolone 0.5–1% fourfold daily.
○ Early discontinuation may cause a rebound recurrence of sterile inflammation.
○ the edge for topical steroid use could also be lower in cases of keratoplasty infection, as they'll reduce the danger of rejection.
Systemic antibiotics
Systemic antibiotics aren't usually given, but could also be appropriate within the following circumstances:
• Potential for systemic involvement, when microbiological/ communicable disease specialist advice should optimally be sought but shouldn't delay treatment:
○ N. meningitidis, during which early systemic prophylaxis could also be life-saving. Treatment is typically with intramuscular benzylpenicillin, ceftriaxone or cefotaxime, or oral ciprofloxacin.
○ H. influenzae infection should be treated with oral amoxicillin with clavulanic acid.
○ N. gonorrhoeae requires a third-generation cephalosporin like ceftriaxone.
• Severe corneal thinning with threatened or actual perforation requires:
○ Ciprofloxacin for its antibacterial activity.
○ A tetracycline (e.g. doxycycline 100 mg twice daily) for its anticollagenase effect.
• Scleral involvement may answer oral or intravenous treatment.
Management of apparent treatment failure
It is important to not confuse ongoing failure of re- epithelialization with continued infection. Drug toxicity, particularly following frequent instillation of fortified amino glycosides, may give increase in discomfort, redness and discharge despite the eradication of infection.
• If no improvement is clear following 24–48 hours of intensive treatment, the antibiotic regimen should be reviewed, including contact with the microbiology laboratory to get the newest report.
• there's no got to change the initial therapy if this has induced a favourable response, albeit cultures show a resistant organism.
• If there's still no improvement after an extra 48 hours, suspension of treatment should be considered for twenty-four hours then re-scraping performed with inoculation on a broader range of media and extra staining techniques requested.