diabetes retinopathy icd 10 | diabetic retinopathy risk factors| diabetic retinopathy on fundoscopy |
diabetic retinopathy treatment injection |diabetic retinopathy stages
_____________________________________________
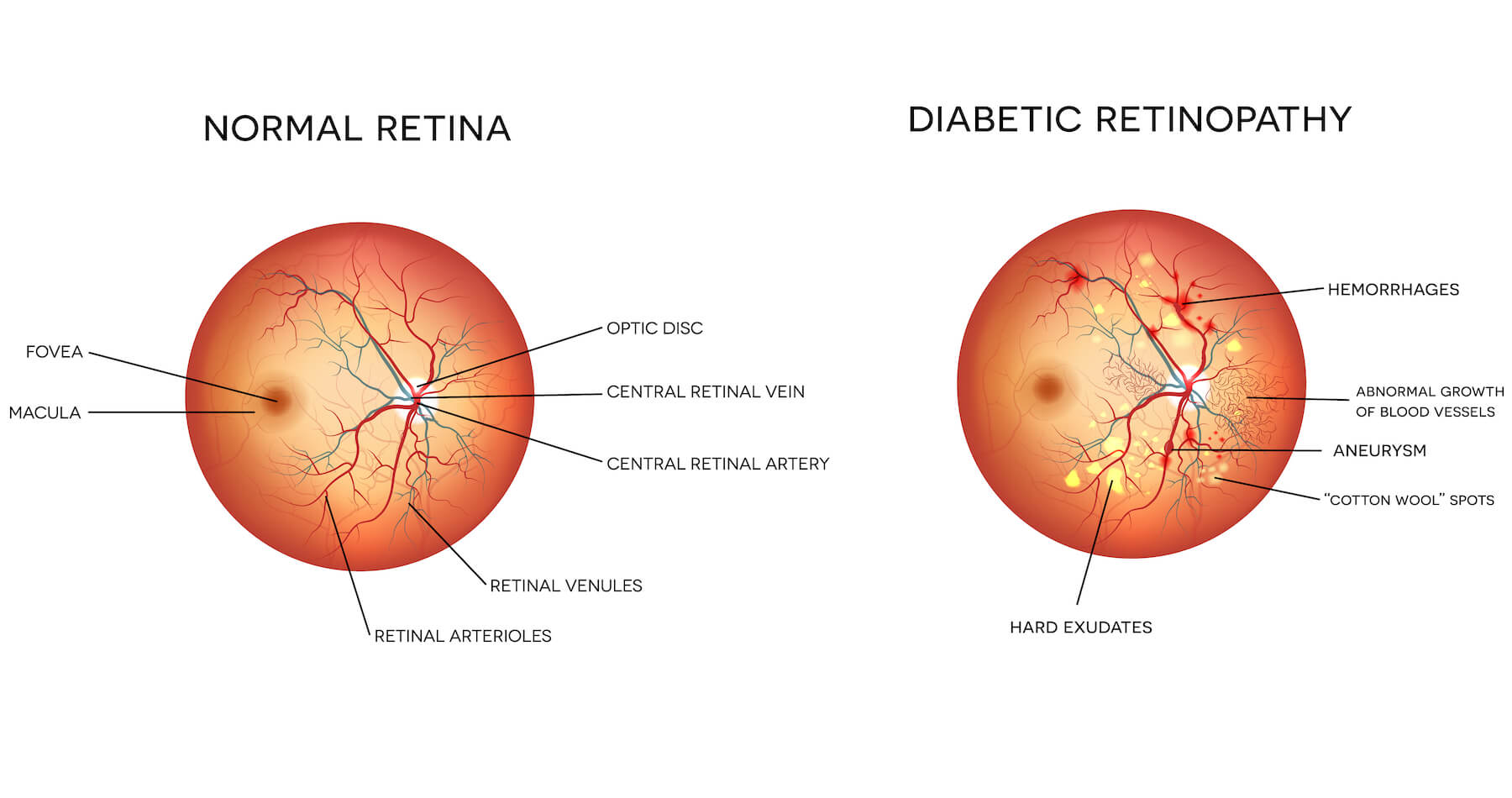
DIABETES RETINOPATHY EYE DISEASE
Diabetes mellitus is the most common cause of blindness among people of working age in the Western world. Two percent of the diabetic population are blind, many of them in the younger age groups. Much of this eye disease can be treated, which makes early identification and referral crucial.
Cataract and primary open angle glaucoma are more common in diabetic than in non-diabetic patients. Cataract can be treated by surgical removal, and primary open angle glaucoma can be treated by drugs and operations that lower the intraocular pressure. Cataract can often be detected by viewing the red reflex; glaucoma by examining the optic disc. It is only too easy to forget to look for glaucomatous cupping of the disc when looking for signs of diabetic retinopathy.
Blinding diabetic retinopathy occurs in both insulin dependent and non-insulin dependent diabetic patients of all ages. For all categories of patient, the longer the duration of the diabetes, the more likely the patient is to have retinopathy (about 80% are affected after 20 years). However, the better the control of blood sugar levels, the lower the incidence of diabetic retinopathy. To avoid missing important signs, diabetic patients should have their fundi examined annually, by dilating the pupils with tropicamide 1%.
Classification of diabetic retinopathy
The current classification of diabetic retinopathy was introduced by the Early Treatment Diabetic Retinopathy Study (ETDRS):
● Non-proliferative diabetic retinopathy (NPDR) mild, moderate, and severe
● Proliferative diabetic retinopathy (PDR)
● Diabetic maculopathy
Non-proliferative diabetic retinopathy
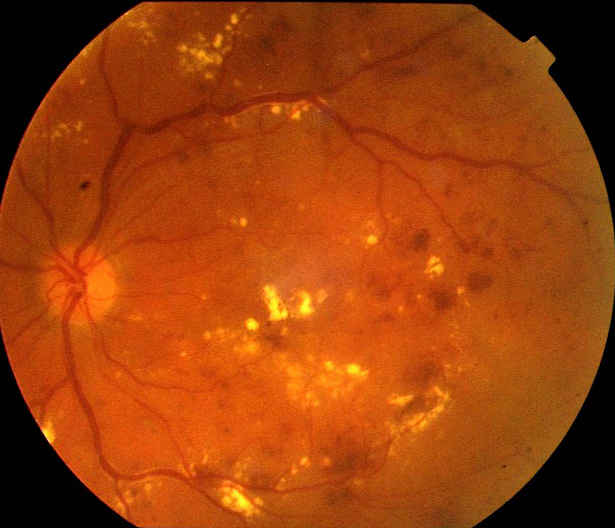
This is typified by microaneurysms, dot haemorrhages, and hard yellow exudates with well defined edges (called background diabetic retinopathy in some classifications).
These changes do not have much effect on vision when they occur in the peripheral retina. However, there is a spectrum of changes in NPDR, some of which are associated with more ischaemic damage. These changes were previously classified as “pre-proliferative” retinopathy. The features of this more ischaemic moderate to severe NPDR are:
● Intraretinal microvascular abnormalities (IRMA)
● Cottonwool spots
● Deeper blotch and cluster haemorrhages
● Venous dilatation, beading and looping.
NPDR may coexist with diabetic maculopathy.
The more ischaemic NPDR changes should alert the clinician to the possibility of progression to blinding proliferative diabetic retinopathy.
Proliferative diabetic retinopathy
Typified by the growth of new vessels on the retina or into the vitreous cavity and thought to result from the ischaemic diabetic retina producing vasoproliferative factors that cause the growth of abnormal new vessels. These vessels may bleed, causing a sudden decrease in vision because of a vitreous haemorrhage. Worse still, this blood often results in the production of contractile membranes that gradually pull off the retina (tractional retinal detachment), causing blindness.
This may occur in any diabetic patient, but more commonly is seen in young, insulin dependent patients. The vision may be 6/6 right up to the moment of a bleed, so early detection of new vessels by adequate fundal examination is crucial. Fluorescein angiography may help to identify areas of retinal ischaemia and new vessel formation. New vessels may also grow at the front of the eye on the iris and occlude the drainage angle of the anterior chamber causing glaucoma (rubeotic glaucoma).
Laser treatment (or any other method of photocoagulation) is used to treat proliferative retinopathy. The laser, however, is not usually used to coagulate new vessels as these may bleed or recur. When a patient has new vessels at the disc, the entire retina is treated with laser, except for the macula area, which preserves the central vision. This treatment, often called “panretinal photocoagulation” or “pattern bombing,” destroys much of the ischaemic peripheral retina and stops it producing the vasoproliferative factors that induce the growth of new vessels, and often the new vessels regress. New blood vessels on the iris that block the outflow of aqueous and cause rubeotic glaucoma may also regress. However, thousands of laser burns and repeated treatments may be needed to achieve this. This treatment may substantially reduce peripheral vision and night vision and means that the patient may have to give up driving.
There is much current research in the development of clinically applicable antagonists to the vasoproliferative growth factors (for example, vascular endothelial growth factor (VEGF) antagonists).
Diabetic maculopathy
Diabetic maculopathy may be divided into four types:
● Focal exudative macular oedema
● Diffuse exudative macular oedema
● Ischaemic maculopathy
● Mixed types.
When diabetic retinopathy causes vessel leakage and ischaemia in the macula area, central vision may be severely affected.
Diabetic maculopathy is the major cause of blindness in maturity onset (Type 2) diabetes, but it also occurs in younger, insulin dependent diabetics. It may be amenable to focal laser photocoagulation, which may help to reduce any leakage, particularly when hard exudates are a prominent feature of the maculopathy.
Screening for diabetic eye disease
Patients may be divided into five groups for screening purposes.
● Patients with no retinopathy or with minimal non-proliferative (background) retinopathy and normal vision when tested with glasses or pinhole. These patients can be reviewed yearly with dilation of the pupils. They should be told to attend sooner if there is a change in vision that is not corrected with glasses.
● Patients with non-proliferative (background) retinopathy and changes around the macula area. They should be referred to an ophthalmologist, as this may herald a blinding maculopathy.
● Patients with non-proliferative (background) retinopathy and impaired acuity not corrected with glasses or pinhole. The patient may have an oedematous or ischaemic form of maculopathy that is extremely hard to diagnose with the direct ophthalmoscope alone. The oedematous form may respond to focal laser treatment if this is given early.
● Patients with moderate to severe non-proliferative (preproliferative) retinopathy. They have no new vessels, but the haemorrhages are larger, the veins are tortuous, and there are cottonwool spots. These signs imply that the retina is ischaemic and that there is a high risk that new vessels will subsequently form. These patients should be referred.
● Patients with proliferative retinopathy. This is typified by new blood vessels, and sometimes cottonwool spots, fibrosis, and vitreous haemorrhages. These patients need immediate referral, particularly if there are vitreous haemorrhages.
In addition to ocular treatment, blood sugar should be carefully controlled. If the blood sugar concentration is brought under control rapidly, the fundus should be reviewed regularly during this period, as there may be a transient worsening of the retinopathy. There is no question that good control of the blood sugar level reduces diabetic retinopathy.
Hypertension, renal failure, and hyperlipidaemia worsen the prognosis of retinopathy and must also be controlled. Patients should be strongly advised not to smoke.
Diabetic patients are also more prone to recurrent corneal abrasions, anteror uveitis, retinal vein occlusions, and cranial nerve palsies.
OPTOMETRY-SHARP VISION
Optometrist