ASTIGMATISM
Astigmatism is a type of refractive error wherein the refraction varies in the different meridia.
Consequently, the rays of light entering in the eye cannot converge to a point focus but form focal lines.
Broadly, there are two types of astigmatism: regular and irregular.
REGULAR ASTIGMATISM
The astigmatism is regular when the refractive power changes uniformly from one meridian to another (i.e., there are two principal meridia).
Etiology
1. Corneal astigmatism is the result of abnormalities of curvature of cornea. It constitutes the most common cause of astigmatism.
2. Lenticular astigmatism is rare. It may be:
i. Curvatural due to abnormalities of curvature of lens as seen in lenticonus.
ii. Positional due to tilting or oblique placement of lens as seen in subluxation.
iii. Index astigmatism may occur rarely due to. variable refractve index of lens in different meridia.
3. Retinal astigmatism due to oblique placement of macula may also be seen occasionally.
Types of regular astigmatism
Depending upon the axis and the angle between the two principal meridia, regular astigmatism can be classified into the following types :
1. With-the-rule astigmatism.
In this type the two principal meridia are placed at right angles to one another but the vertical meridian is more curved than the horizontal. Thus, correction of this astigmatism will require the concave cylinders at 180° ± 20° or convex cylindrical lens at 90° ± 20°.
This is called 'with-the-rule' astigmatism, because similar astigmatic condition exists normally (the vertical meridian is normally rendered 0.25 D more convex than the horizontal meridian by the pressure of eyelids).
2. Against-the-rule astigmatism
refers to an astigmatic condition in which the horizontal meridian is more curved than the vertical meridian.
Therefore, correction of this astigmatism will require the presciption of convex cylindrical lens at 180° ± 20° or concave cylindrical lens at 90° ± 20° axis.
3. Oblique astigmatism
It is a type of regular astigmatism where the two principal meridia are not the horizontal and vertical though these are at right angles to one another (e.g., 45° and 135°).
Oblique astigmatism is often found to be symmetrical (e.g. cylindrical lens required at 30° in both eyes) or complementary (e.g., cylindrical lens required at 30° in one eye and at 150° in the other eye).
4. Bioblique astigmatism.
In this type of regular astigmatism the two principal meridia are not at right angle to each other e.g., one may be at 30o and other at 100°.
Optics of regular astigmatism
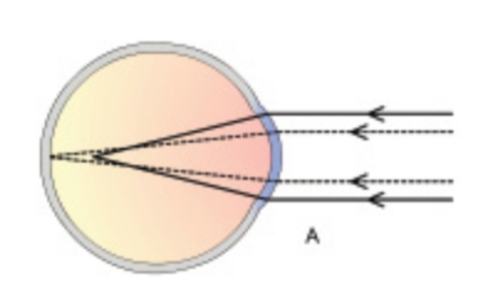
As already mentioned, in regular astigmatism the parallel rays of light are not focused on a point but form two focal lines.
The configuration of rays refracted through the astigmatic surface (toric surface) is called Sturm’s conoid and the distance between the two focal lines is known as focal interval of Sturm.
The shape of bundle of rays at different levels.
Refractive types of regular astigmatism
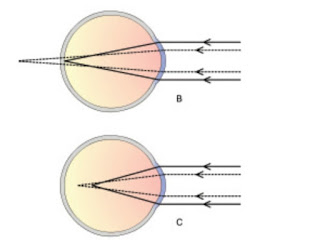
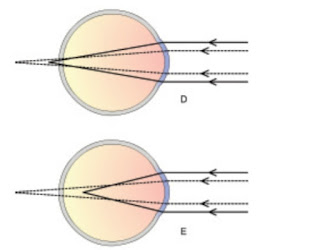
Depending upon the position of the two focal lines in relation to retina, the regular astigmatism is further
classified into three types:
1. Simple astigmatism,
wherein the rays are focused on the retina in one meridian and either in front (simple myopic astigmatism ) or behind (simple hypermetropic astigmatism ) the retina in the other meridian.
2. Compound astigmatism.
In this type the rays of light in both the meridia are focused either in front or behind the retina and the condition is labelled as compound myopic or compound hypermetropic astigmatism, respectively.
3. Mixed astigmatism refers to a condition wherein the light rays in one meridian are focused in front and in other meridian behind the retina.
Thus in one meridian eye is myopic and in another hypermetropic. Such patients have comparatively less symptoms as 'circle of least diffusion' is formed on the retina.
Symptoms
Symptoms of regular astigmatism include:
(i) defective vision;
(ii) blurring of objects;
(iii) depending upon the type and degree of astigmatism, objects may appear proportionately elongated; and
(iv) asthenopic
symptoms, which are marked especially in small amount of astigmatism, consist of a dull ache in the eyes, headache, early tiredness of eyes and sometimes nausea and even drowsiness.
Signs
1. Different power in two meridia is revealed on retinoscopy or autorefractometry.
2. Oval or tilted optic disc may be seen on ophthalmoscopy in patients with high degree of astigmatism.
3. Head tilt. The astigmatic patients may (very exceptionally) develop a torticollis in an attempt to bring their axes nearer to the horizontal or vertical meridians.
4. Half closure of the lid. Like myopes, the astigmatic patients may half shut the eyes to achieve the greater clarity of stenopaeic vision.
Investigations
1. Retinoscopy reveals different power in two different axis
2. Keratometry.
Keratometry and computerized corneal topotograpy reveal different corneal curvature in two different meridia in corneal astigmatism.
3. Astigmatic fan test and
4. Jackson's cross cylinder test.
These tests are useful in confirming the power and axis of cylindrical lenses.
Treatment
1. Optical treatment of regular astigmatism comprises the prescribing appropriate cylindrical lens, discovered after accurate refraction.
i. Spectacles with full correction of cylindrical power and appropriate axis should be used for distance and near vision.
ii. Contact lenses.
Rigid contact lenses may correct upto 2-3 of regular astigmatism, while soft contact lenses can correct only little astigmatism.
For higher degrees of astigmatism toric contact lenses are needed. In order to maintain the correct axis of toric lenses, ballasting or truncation is required.
2. Surgical correction of astigmatism is quite effective.
Refractive surgery for astigmatism
Refractive surgical techniques employed for myopia can be adapted to correct astigmatism alone or simultaneously with myopia as follows:
1. Astigmatic keratotomy (AK) refers to making transverse cuts in the mid periphery of the steep corneal meridian. AK can be performed alone (for astigmatism only) or along with RK.
2. Photo-astigmatic refractive keratotomy (PARK) is performed using excimer laser.
3. LASIK procedure can also be adapted to correct astigmatism upto 5D.
Management of post-keratoplasty astigmatism
1. Selective removal of sutures in steep meridians may improve a varying degree of astigmatism and should be tried first of all.
2. Arcuate relaxing incisions in the donor cornea along the steep meridian may correct astigmatism up to 4-6 D.
3. Relaxing incisions combined with compression sutures may correct astigmatism up to 10 D.
4. Corneal wedge resection with suture closure of the wound may be performed in the flat meridian to correct astigmatism greater than 10 D.
5. LASIK procedure can also be adopted to correct post-keratoplasty astigmatism.
OPTOMETRY-SHARP VISION
Optometrist