What is Myopia ?
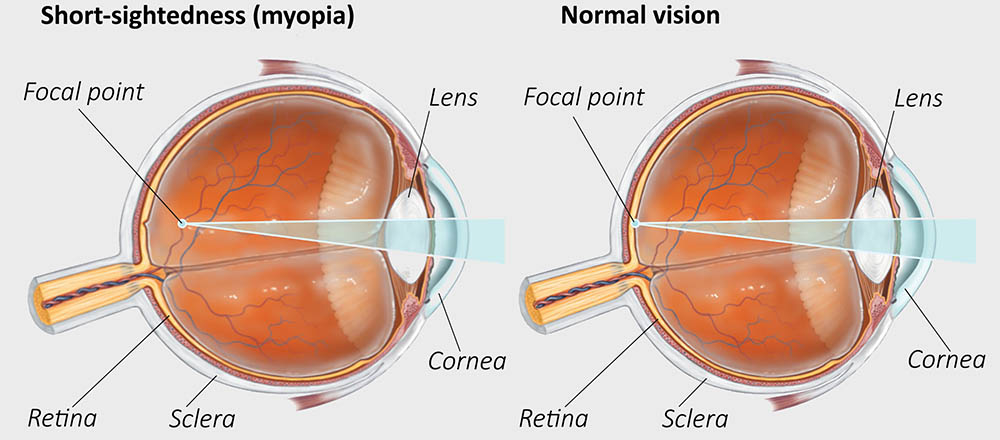
Myopia or short-sightedness is a type of refractive error in which parallel rays of light coming from infinity are focused in front of the retina when
accommodation is at rest.
Etiological classification
1. Axial myopia results from increase in antero- posterior length of the eyeball. It is the commonest form.
2. Curvatural myopia occurs due to increased curvature of the cornea, lens or both.
3. Positional myopia is produced by anterior placement of crystalline lens in the eye.
4. Index myopia results from increase in the refractive index of crystalline lens associated with nuclear sclerosis.
5. Myopia due to excessive accommodation occurs in patients with spasm of accommodation.
Clinical varieties of myopia
1. Congenital myopia
2. Simple or developmental myopia
3. Pathological or degenerative myopia
4. Acquired myopia which may be:
(i) post-traumatic
(ii) post-keratitic
(iii) drug-induced
(iv)pseudomyopia
(v) space myopia
(vii) night myopia
(viii) consecutive myopia.
1. Congenital myopia
Congenital myopia is present since birth, however, it is usually diagnosed by the age of 2-3 years. Most of the time the error is unilateral and manifests as anisometropia. Rarely, it may be bilateral. Usually the error is of about 8 to 10 which mostly remains constant. The child may develop convergent squint in order to preferentially see clear at its far point (which is about 10-12 cms).
Congenital myopia may
sometimes be associated with other congenital anomalies such as cataract, microphthalmos, aniridia, megalocornea, and congenital separation of retina.
Early correction of congenital myopia is desirable.
2. Simple myopia Simple or developmental myopia is the commonest variety.
It is considered as a physiological error not associated with any disease of the eye. Its prevalence increases from 2% at 5 years to 14% at 15 years of age. Since the sharpest rise occurs at school going
age i.e., between 8 year to 12 years so, it is also called school myopia.
Etiology.
It results from normal biological variation in the development of eye which may or may not be genetically determined. Some factors associated with simple myopia are as follows:
*� Axial type of simple myopia may signify just a physiological variation in the length of the eyeball or it may be associated with precocious neurological growth during childhood.
*� Curvatural type of simple myopia is considered to be due to underdevelopment of the eyeball.
�* Role of diet in early childhood has also been reported without any conclusive results.
*� Role of genetics. Genetics plays some role in the biological variation of the development of eye, as prevelance of myopia is more in children with
both parents myopic (20%) than the children with one parent myopic (10%) and children with no parent myopic (5%).
�* Theory of excessive near work in childhood was also put forward, but did not gain much importance. In fact, there is no truth in the folklore
that myopia is aggravated by close work, watching television and by not using glasses.
Clinical picture
Symptoms
�* Poor vision for distance (short-sightedness) is the main symptom of myopia.
�
* Asthenopic symptoms may occur in patients with
small degree of myopia.
�* Half shutting of the eyes may be complained by parents of the child. The child does so to achieve the greater clarity of stenopaeic vision.
Signs
*� Prominent eyeballs. The myopic eyes typically are large and somewhat prominent.
*� Anterior chamber is slightly deeper than normal.
�
* Pupils are somewhat large and a bit sluggishly reacting.
�
* Fundus is normal; rarely temporal myopic crescent may be seen.
� Magnitude of refractive errror.
Simple myopia usually occur between 5 and 10 year of age and it keeps on increasing till about 18-20 years of age at a rate of about –0.5 ± 0.30 every year. In simple myopia, usually the error does not exceed 6 to 8. Diagnosis is confirmed by performing retinoscopy.
3. Pathological myopia
Pathological/degenerative/progressive myopia, as the name indicates, is a rapidly progressive error which starts in childhood at 5-10 years of age and results in high myopia during early adult life which is usually associated with degenerative changes in the eye.
Etiology.
It is unequivocal that the pathological myopia results from a rapid axial growth of the eyeball which is outside the normal biological variations of development. To explain this spurt in axial growth various theories have been put forward. So far no satisfactory hypothesis has emerged to explain the
etiology of pathological myopia.
However, it is definitely linked with
(i) heredity and
(ii) general growth process.
1. Role of heredity. It is now confirmed that genetic factors play a major role in the etiology, as the progressive myopia is
(i) familial
(ii) more common in certain races like Chinese, Japanese, Arabs and Jews
(iii) uncommon among Negroes, Nubians and Sudanese. It is presumed that heredity-linked growth of retina is the determinant in the development of myopia.
The sclera due to its distensibility follows the retinal growth but the choroid undergoes degeneration due to stretching, which in turn causes degeneration of retina.
2. Role of general growth process, though minor, cannot be denied on the progress of myopia.
Lengthening of the posterior segment of the globe commences only during the period of active growth and probably ends with the termination of the active growth.
Therefore, the factors (such as nutritional deficiency, debilitating diseases, endocrinal disturbances and indifferent general health) which affect the general growth process will also influence the progress of myopia.
Clinical picture
Symptoms
1. Defective vision. There is considerable failure in visual function as the error is usually high. Further, due to progressive degenerative changes, an uncorrectable loss of vision may occur.
2. Muscae volitantes i.e., floating black opacities in front of the eyes are also complained of by many patients. These occur due to degenerated liquified vitreous.
3. Night blindness may be complained by very high myopes having marked degenerative changes.
Signs
1. Prominent eye balls. The eyes are often prominent, appearing elongated and even simulating an exophthalmos, especially in unilateral cases. The elongation of the eyeball mainly affects the posterior pole and surrounding area; the part of the eye anterior to the equator may be normal.
2. Cornea is large.
3. Anterior chamber is deep.
4. Pupils are slightly large and react sluggishly to light.
5. Fundus examination reveals following
characteristic signs :
(a) Optic disc appears large and pale and at its temporal edge a characteristic myopic crescent is present.
Sometimes peripapillary crescent encircling the disc may be present, where the choroid and retina is distracted away from the disc margin.
A super-traction crescent (where the retina is pulled over the disc margin) may be present on the nasal side.
(b) Degenerative changes in retina and choroid are common in progressive myopia.
These are characterised by white atrophic patches at the macula with a little heaping up of pigment around them. Foster-Fuchs' spot (dark red circular patch due to sub retinal neovas-cularization and choroidal haemorrhage) may be present at the macula.
Cystoid degeneration may be seen at the periphery. In an advanced case there occurs total retinal atrophy, particularly in the central area.
(c) Posterior staphyloma due to ectasia of sclera at posterior pole may be apparent as an excavation with the vessels bending backward over its margins.
(d) Degenerative changes in vitreous include: liquefaction, vitreous opacities, and posterior vitreous detachment (PVD) appearing as Weiss' reflex.
6. Visual fields show contraction and in some cases ring scotoma may be seen.
7. ERG reveals subnormal electroretinogram due to chorioretinal atrophy.
Complications
(i) Retinal detachment
(ii) complicated cataract
(iii) vitreous haemorrhage
(iv) choroidal haemorrhage
(v) Strabismus fixus convergence.
Treatment of myopia
1. Optical treatment of myopia constitutes prescription of appropriate concave lenses, so that clear image is formed on the retina.
The basic rule of correcting myopia is converse of that in hypermetropia, i.e., the minimum acceptance providing maximum vision should be prescribed. In very high myopia under correction is always better to avoid the problem of near vision and that of minification of images.
Modes of prescribing concave lenses are spectacles and contact lenses.
Contact lenses are particularly justified in cases of high myopia as they avoid peripheral distortion and minification produced by strong concave spectacle lens.
2. Surgical treatment of myopia is becoming very popular now-a-days.
3. General measures empirically believed to effect the progress of myopia (unproven usefulness) include balanced diet rich in vitamins and proteins and early management of associated debilitating disease.
4. Low vision aids (LVA) are indicated in patients of progressive myopia with advanced degenerative changes, where useful vision cannot be obtained with spectacles and contact lenses.
5. Prophylaxis (genetic counselling). As the pathological myopia has a strong genetic basis, the hereditary transfer of disease may be decreased by advising against marriage between two individuals with progressive myopia. However, if they do marry, they should not produce children.
OPTOMETRY-SHARP VISION
Optometrist
Tags:
Refractive error